Secretion
Insulin hormone is secreted from the pancreas as an endocrine function. The beta cells of islets of Langerhans of the pancreas release insulin with the stimulus of an increase in glucose.

There is the secretion of Glucagon by alpha cells, Insulin by beta cells, and somatostatin by delta cells of islets of Langerhans of the pancreas. These secreted hormones have a local effect on the regulation of each other secretion shown in the diagram below.
Glucagon has a stimulatory effect on both beta cells (insulin) and delta cells (somatostatin).
Insulin has an inhibitory effect on alpha cells that secrete glucagon.
Somatostatin has an inhibitory effect on both alpha cells and beta cells.

Mechanism of insulin secretion from the beta cell of islets of Langerhans
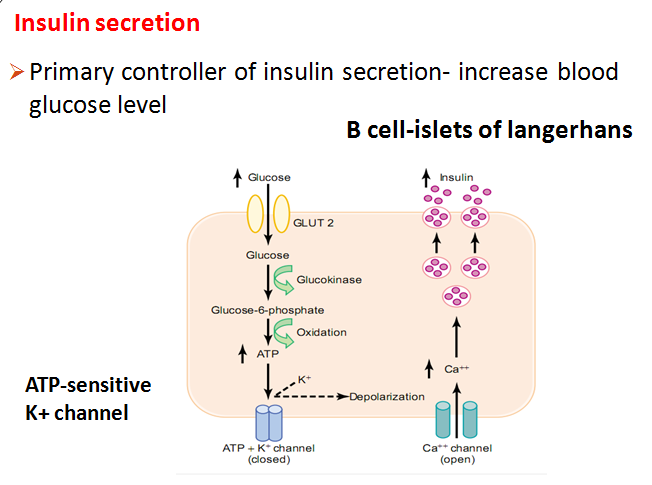
An increase in glucose level is sensed by beta cells – glucose is moved inside the cell by GLUT 2 channel and glycolysis takes place – release of ATP inside the cell that blocks ATP-dependent potassium channels- potassium is accumulated inside the cell increase its potential and depolarization of cell take place- depolarization cause entry of calcium – increase in calcium inside the cell cause release of insulin hormone by exocytosis process.
Function of insulin
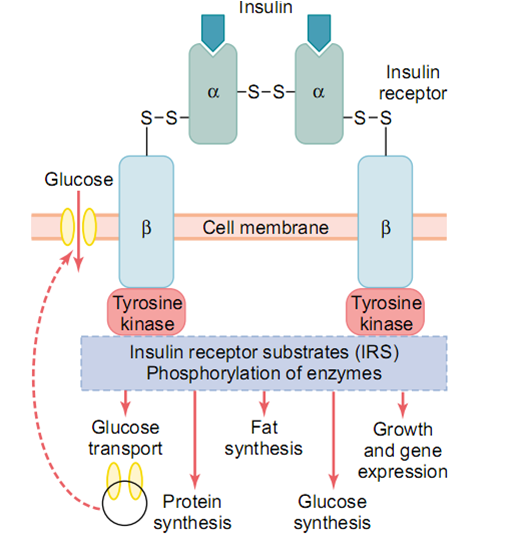
It is an anabolic hormone. For the action of the insulin it binds with the tyrosine kinase receptor in the target cell- phosphorylation of enzymes that will cause different functions like fat synthesis, protein synthesis, and glucose synthesis. In simple language, it provides all the raw materials needed for fat synthesis, protein synthesis, and so on.
Effects of Insulin on carbohydrate metabolism
After meals increase glucose uptake by peripheral tissues (skeletal muscle & adipose tissue by GLUT 4 channels by the action of insulin). There is the new formation and translocated of already formed GLUT 4 channels in the cell membrane of skeletal muscle and adipose tissue for the entry of glucose inside the cell and decrease the blood glucose level.
Note: In exercise conditions, there is entry of glucose inside the skeletal muscle without the help of insulin. This is the reason, why exercise is important in diabetes mellitus.

•In muscle- glucose is stored in glycogen
•In the liver- promote glycogen synthesis
•Excess glucose- converse into FA- packaged as triglyceride- transported & store in adipose tissue
•Inhibit gluconeogenesis- inhibiting gluconeogenic enzymes
•Net effect- increase glycogen stored in the liver (100 gms), decrease glucose output
Effects of Insulin on fat metabolism
Increase fat synthesis
In the liver, excess carbohydrates- provide a substrate for fat synthesis.
store fat in adipose tissue
Effect of Insulin on protein metabolism
Transport amino acids into cells translation of mRNA, rate of transcription of selected DNA genetic sequence
Decrease rate of amino acid release from muscles & extrahepatic tissue
Net effect- promotes protein synthesis & inhibits protein catabolism
Regulation of insulin secretion
Secretion of insulin is stimulated by increased blood glucose levels, for example after eating a
meal, and to a lesser extent by parasympathetic stimulation, raised blood amino acid and fatty acid levels, and gastrointestinal hormones, e.g. gastrin, secretin, and cholecystokinin.
Secretion is decreased by sympathetic stimulation, glucagon, adrenaline, cortisol, and somatostatin which is secreted by the hypothalamus and pancreatic islets.
Factors/Conditions that increase or decrease insulin secretion
Increase Insulin Secretion
•Increased blood glucose**
•Increased blood free fatty acids
•Increased blood amino acids
•GIT hormones – gastrin
•Glucagon, growth hormone, cortisol
•β-Adrenergic stimulation
•Insulin resistance; obesity
•Sulfonylurea drugs (glyburide, tolbutamide)
Decrease Insulin Secretion
•Decreased blood glucose
•Fasting
•Somatostatin
•α-Adrenergic activity
•Leptin


