Parathyroid (PTH) and calcitonin hormones play major roles in homeostasis of the calcium and phosphorus. Overall the parathyroid hormone increases the calcium level in the blood whereas calcitonin decreases the calcium level in the blood plasma. Without calcitonin also parathyroid hormone can maintain the calcium level in the blood. As the body decreases the parathyroid hormone secretion when there are large amounts of calcium and vice versa.
Importance of calcium and phosphorus in the body
Ca2+= 2nd messenger, necessary for blood coagulation, muscle contraction,& nerve function, structural role in hard tissues (bone & teeth)
Phosphate= found in ATP, cAMP, 2,3-diphosphoglycerate; phosphorylation & dephosphorylation of proteins, lipids & 2nd messenger-key regulatory steps in metabolic & signaling pathways; the backbone of nucleic acid.
Synthesis of parathyroid hormone
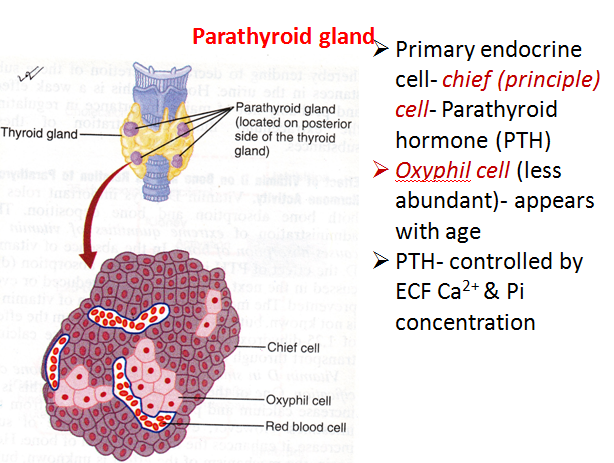
•PTH is synthesized and secreted by the parathyroid gland which lies posterior to the thyroid glands.
•The blood supply to the parathyroid glands is from the thyroid arteries.
•The Chief Cells in the parathyroid gland are the principal site of PTH synthesis.
Regulation of Parathyroid hormone
•The dominant regulator of PTH is plasma Ca2+.
•Secretion of PTH is inversely related to [Ca2+].
•Maximum secretion of PTH occurs at plasma Ca2+ below 3.5 mg/dL.
•At Ca2+ above 5.5 mg/dL, PTH secretion is maximally inhibited.
•PTH secretion responds to small alterations in plasma Ca2+ within seconds.
•A unique calcium receptor within the parathyroid cell plasma membrane senses changes in the extracellular fluid concentration of Ca2+.
Functions of Parathyroid Hormones
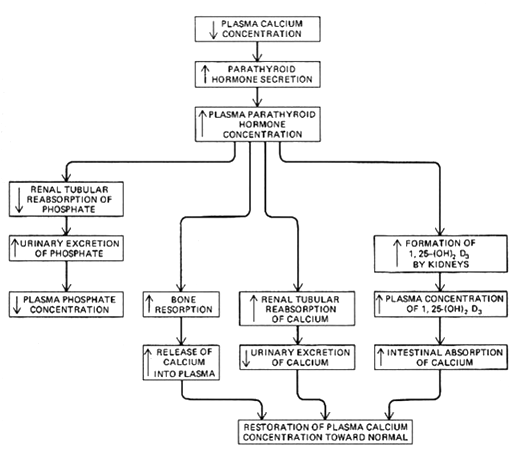
•The overall action of PTH is to increase plasma Ca++ levels and decrease plasma phosphate levels.
•PTH acts directly on the bones to stimulate Ca++ resorption and kidney to stimulate Ca++ reabsorption in the distal tubule of the kidney and to inhibit the reabsorption of phosphate (thereby stimulating its excretion).
•PTH also acts indirectly on the intestine by stimulating 1,25-(OH)2-D synthesis for the absorption of Ca++.
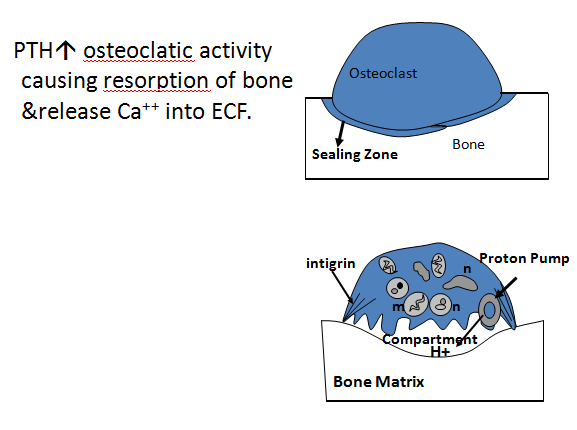
Bone resorption: Parathyroid hormone acts on the osteoclastic cell of the bone and releases hydrogen ions in that region and dissolves the bone.
Female hormone prevents somehow this action of the Parathyroid hormone and this is the reason for osteoporosis in menopausal women where there is a lack of estrogen hormone.
Calcitonin hormone
•Calcitonin acts to decrease plasma Ca++ levels.
•While PTH and vitamin D act to increase plasma Ca++— only calcitonin causes a decrease in plasma Ca++.
•Calcitonin is synthesized and secreted by the parafollicular cells of the thyroid gland.
•They are distinct from thyroid follicular cells by their large size, pale cytoplasm, and small secretory granules.
•The major stimulus of calcitonin secretion is a rise in plasma Ca++ levels
•Calcitonin is a physiological antagonist to PTH with regard to Ca++ homeostasis
•The target cell for calcitonin is the osteoclast.
•Calcitonin acts to inhibit osteoclast activity
•The major effect of calcitonin administration is a rapid fall in Ca2+ caused by the inhibition of bone resorption.
Vitamin D
secretion of vitamin D in the skin from the effect of sunlight then in the kidney and convert to the active form of vitamin D (1,25 dihydro cholecalciferol).
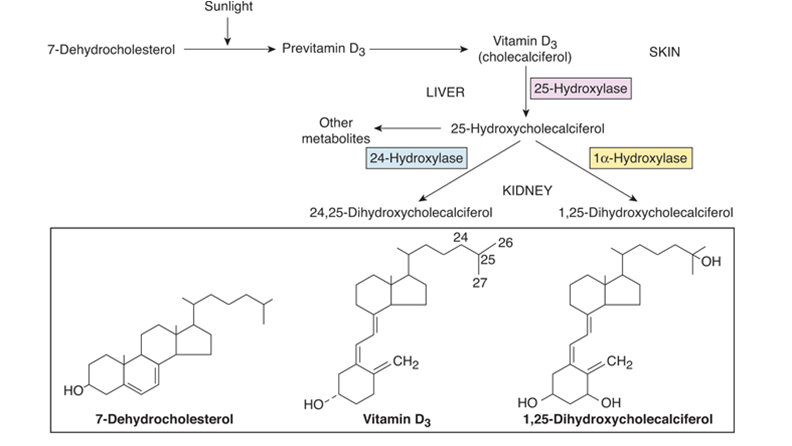
Functions of Vitamin D
1,25-dihydroxyvit. D= facilitates Ca2+ and Pi (Phosphorus)reabsorption in kidneys;
Increases the synthetic activity of osteoblasts & is necessary for the calcification of matrix
PTH affects Ca2+ absorption in the gut indirectly by stimulating renal 1α-hydroxylase activity
A summary of the role of the Parathyroid hormone and Vitamin D is shown below in the diagram